고정 헤더 영역
상세 컨텐츠
본문
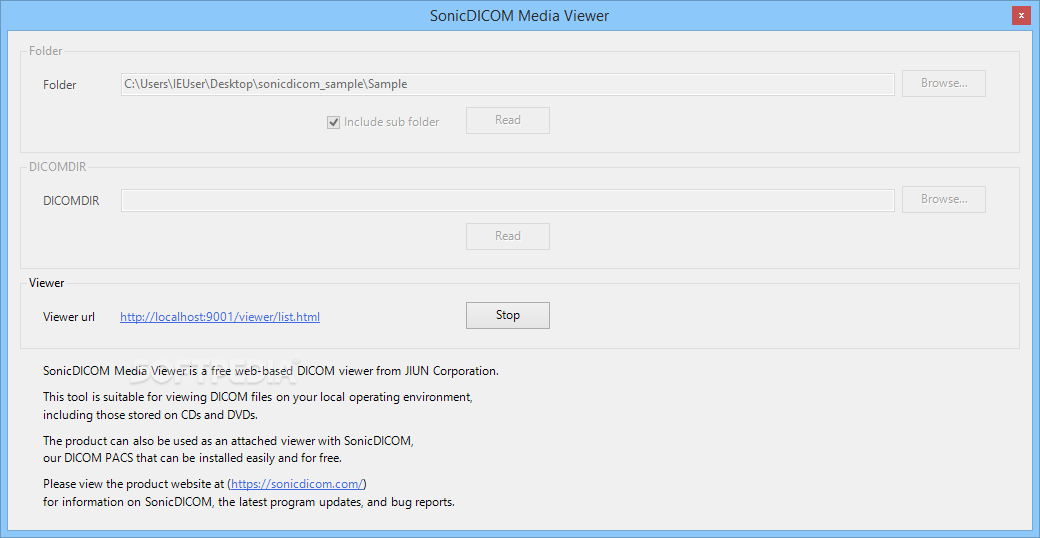
Sample dataListed below are the anonymized data sets available for download. Many of the DICOM data sets are also available on the. Datasets marked LEE are in Little Endian Explicit Transfer Syntax (1.2.840.10008.1.2.1); those marked JPG are in JPEG2000 Transfer Syntax (1.2.840.10008.1.2.4.90). This syntax uses image compression and can result in image files that are considerably smaller (up to 10 times smaller). However not all imaging software can read images with JPEG2000 image compression.You may also wish to visit:. A single data set converted in multiple ways.Sample data on I Do Imaging. Browser viewer links are hosted on server.
Previous studies suggests that cone beam computerized tomography (CBCT) images could provide reliable information regarding the fate of bone grafts in the maxillofacial region, but no systematic information regarding the standardization of CBCT settings and properties is available, i.e., there is a lack of information on how the images were generated, exported, and analyzed when bone grafts were evaluated. The aim of this study was to (1) do a systematic review on which type of CBCT-based DICOM images have been used for the evaluation of the fate of bone grafts in humans and (2) use a software suggested in the literature to test DICOM-based data sets, exemplifying the effect of variation in selected parameters (windowing/contrast control, plane definition, slice thickness, and number of measured slices) on the final image characteristics. The results from review identified three publications that used CBCT to evaluate maxillofacial bone grafts in humans, and in which the methodology/results comprised at least one of the expected outcomes (image acquisition protocol, image reconstruction, and image generation information). The experimental shows how the influence of information that was missing in the retrieved papers, can influence the reproducibility and the validity of image measurements.
Although the use of CBCT-based images for the evaluation of bone grafts in humans has become more common, this does not reflect on a better standardization of the developed studies. Parameters regarding image acquisition and reconstruction, while important, are not addressed in the proper way in the literature, compromising the reproducibility and scientific impact of the studies. IntroductionBone volume and bone quality are factors of particular interest in determining the optimal location for placing dental implants and for their prognosis over time. Material and MethodsThe MEDLINE (PubMed) bibliographic database was searched from 1950 to October 2010 for reports on the use of cone beam CT images for the evaluation of bone grafts. Review Search ResultsThe search strategy yielded 527 publications in MEDLINE (PubMed). “Hand” search did not reveal any additional papers.
StudySample characteristicsNumber of patientsAge range (years)Type of graftNumber of examinationsPeriod of examinationHamada et al. 2005 13 (6 males/7 females)8–38Onlay (does not specify from where the blocks were retrieved)1Between 2 and 51 months post-surgeryGapski et al. 2008 1 (female)53Inlay (bovine hydroxyapatite and bone allograft)3Baseline, immediate post-operative and 6-month controlOberoi et al. 2009 21 (15 males/6 females)7–13Onlay (blocks retrieved from the iliac crest)2Baseline and a minimum of 12 months after surgery. StudyImage reconstruction protocolDICOM orientation softwareImage rendering softwareDirect measurement/exported imageResolutionWindowingPlane orientation definitionMeasured slicesSlice thicknessHamada et al. 2005 VIP station imaging (Cemax-Icon Inc., Fremont, USA)Not usedDirect measurementImages not exportedndBased on central panoramic curve of each subject, and subsequent sections based on that curve7 (1 central, 3 buccal, and 3 palatal)1.0 mmGapski et al.
2008 ndICATVision (Imaging Sciences International, Hatfield, USA)Direct measurementImages not exportedndndndndOberoi et al. 2009 CB Works 2.01 (CyberMed Inc., Seoul, Korea)Amira 3.1.1 (Visage Imaging, USA)Direct measurementImages not exportedndFive well-defined planes delimitating a ROI, in which the sections were analyzedAll from the ROI0.4 mm. The studies differed notably with respect to image acquisition, generation, and reconstruction.
In total, the included papers reported the fate of the graft in 35 patients using CBCT as the evaluation method –.All patients had alveolar defects located in the maxilla, 34 of them in the anterior region (onlay bone grafts) and one in the posterior (sinus lift—“inlay” bone graft). In one study, autologous bone retrieved from the anterior iliac crest was used as grafting material , and one study used a mix of bovine hydroxyapatite and bone allograft. The third study did not report the origin of the grafts.Two studies had a baseline image to be compared with the final image , , and the only study with a fixed evaluation interval was the case report.
One study reported complete information regarding the image acquisition protocols (acquisition time, kilovoltage (kV), miliampere (mA), image resolution, and slice thickness).All studies were based on measurements made directly in the DICOM rendering software, but none of them reported information regarding the windowing (contrast control), which was used to visualize bone. Two studies displayed information on how the orientation plane for generation of image sections was defined, and also how the sections were oriented, and how many sections were evaluated ,.The three studies used different software to reorient and render the DICOM files.
One study was based on software that runs an exclusive file extension (ICATVision), i.e., the DICOM files were converted to another format before the images were accessed and measured. The other two were based on DICOM manipulating software; only one of which is still available on the market (Amira, Visage Imaging Inc., USA). This piece of software was therefore chosen for the next phase of our study. WindowingNone of the selected papers described this issue. The used software does not predefine specific values for different types of tissue, but allows the user to change the values, and therefore the view, to the image’s mapped values. Plane DefinitionThe selected software does not allow the creation of individualized planes for image segmentation. This made it more difficult to find the correct sections that would intercept the evaluated region perpendicularly.
Therefore, it is complex to obtain standardized transversal slices of the region of interest (ROI), which will become a problem when measuring graft height and width.In Fig., the same ROI is shown in different planes. The ROI is from the posterior maxilla, and the correct transverse section of the area to be grafted can be seen in the coronal plane (a), while the sagittal plane (c) shows an image, which is useless for height and width assessment. In the anterior region, the transverse sections (perpendicular to the evaluated region) are found on the sagittal plane as shown in Fig. The ideal software should facilitate the creation of individualized new planes allowing the generation of exact bucco-palatal transverse images of the graft. Section ThicknessIn the selected software, the module that allows image segmentation and windowing does not allow changes in section thickness. The voxel resolution is therefore the thickness of the displayed section.
Although restrictive, image standardization can be achieved in this way. Another module in the software (Multi-planar Viewer) allows section thickness manipulation, but is not connected to windowing adjustment. To exemplify how section thickness modification can influence the characteristics of the final image, Fig. Illustrates images of the same region generated using different section thickness values, ranging from 0.25 to 10 mm. Test anterior grafted region displayed using different values for section thickness (the figure on the top left)The subjective evaluation of these images reveals that the thickness of the sections affects the appearance of the reconstructed image, e.g., superimposition of anatomic structures and bone grafts/screws is seen in thick sections.
This “anatomical noise” can disturb images interpretation. This is illustrated in Fig., with a thick section (30 mm) providing a final image in which it is impossible to delineate grafts placed at different sites. Number of SectionsWe generated a set of images of a grafted region at three different time periods: baseline (before grafting procedure), immediately after surgery, and 6 months post-operatively. The images were acquired using a windowing definition able to show transverse (sagittal) sections ( W = 3,086 and L = 667), the section thickness was 0.25 mm and the interval between the sections was 1.0 mm, until a complete mapping of the grafted block was fulfilled.Figure shows that different results are obtained if only a central image of the graft is used to measure height and width compared to the information shown on sections 4D and 4E with their adjacent sections, such as 4A/4B and 4G/4H. When comparing the same grafted region at different time periods, the ideal should be to obtain a full profile of the bone area, allowing the visualization of the final “volume” of the area (complete width and height profile).
DiscussionThe success rate associated with dental implant treatment is directly related to the bone volume and quality surrounding the implants, and therefore special attention has been given in the literature to bone-grafting procedures and how to evaluate the fate of the grafts –,. Previous literature has agreed on histology as the “gold standard” evaluation method to evaluate bone graft remodeling, but an alternative method could be non-invasive imaging –,.A new imaging method for dentistry, CBCT has enabled 3D display of bone structures, which facilitates the assessment of boundaries of bone in areas selected for implant placement ,. The possibility of 3D manipulation and segmentation of the generated images has increased the value of this method. The parameters can be varied in order to attain images of the region(s) of interest, ranging from section thickness to the mapping of scalar values stored with the image that will be shown to the user (windowing, or contrast control) ,.Data transfer between workstations connected to a CBCT scanner follows the DICOM standard protocol ,. DICOM packages include information regarding patient information, image acquisition, and the list of images that correspond to axial sections to form 3D images, allied to a “map” of how the images must be oriented to generate the final images. The CBCT manufacturers provide software to generate DICOM files of the exams, but there is also a wide range of software able to import DICOM files, work on them, and export sections of images in other formats , , and those images can later be used for various measurements. A major problem is, however, that the selection of parameters related to image generation and manipulation in CBCT imaging, including the selection of software, cross-sectional slice thickness, inter-slice interval, windowing (contrast control), and resolution, seems to have been performed almost arbitrarily.The intention of our review was to recapitulate how human bone grafts have been evaluated in studies using CBCT-based DICOM data sets and illustrate the deficiencies associated with the lack of standardization.
In the systematic review, three publications were identified that used a CBCT technique to evaluate maxillofacial bone grafts in humans, together with at least one of the outcomes under review (image acquisition protocol, image reconstruction, and generation information) –. Included papers reported the outcomes of 35 maxillary grafted patients. The way images were acquired, generated, and reconstructed differed notably in these studies, and only one study provided complete information for image acquisition (time, kV, mA, and resolution).
This information is extremely relevant in order to compare studies in the literature since these parameters can directly influence the characteristics of the final images. The imaging protocol should concern population dose and image quality.
The estimation of fatal cancer risk arising from oral and maxillofacial CBCT imaging has increased from 23% to 224% following new recommendations for calculating effective dose , and radiation dose is directly connected to the acquisition time, along with other factors such as FOV, mA, and kV. It is important to emphasize that the “ALARA” principle should always be applied, thus the protocol (i.e., radiation dose) must be tailored to each case. The majority of the screened studies did not provide complete information regarding these variables.
However, standardization over time is essential, since after windowing and leveling adjustments technique artifacts and noise may be minimized by software manipulation.Pertaining to image quality, the literature still lacks evidence since no studies seem to have been conducted on the relationship between dose and quality for CBCT. Studies on medical CT scanning are not comparable with CBCT since the resolution of the CBCT devices used in dentistry is higher, with small voxel sizes and also with a different signal-to-noise-pixel size correlation, derived from quantum statistics. The structural details of a CBCT-based image are directly related to the voxel size, and depending on the purpose of the images, this may play a decisive role.
No information regarding the effects of different voxel sizes on the evaluation of bone grafts was found in the literature.All selected papers concluded on results from measurements made directly in the image rendering software or in the DICOM orientation software; however, they were poor in presenting how the images were generated. The first point to address is the contrast control of the displayed image, also known as “windowing”. For DICOM images, visualization is based on a threshold filter, which assigns a binary value, either transparent or visible, to each voxel based on its gray level value. For most DICOM orientation software, the user is able to define the critical value that splits the voxels into visible and invisible, or, in other words, the windowing of the image. This result in a rendered image is composed of all visible voxels.
As shown by our test images, different windowing values provide different final images when different values for the center level ( L) and band width ( W) of shades of gray are used. This may influence linear and volumetric measurements.Cortical bone, bone trabeculae, and intertrabecular tissue have varying densities, and in traditional medical CT these different densities can be interpreted using HU, providing a quantitative assessment of bone density as measured by its ability to attenuate an X-ray beam. However, density differences present a challenge when examining CBCT images. The displayed grey levels in CBCT systems are arbitrary and do not allow for the assessment of bone quality as performed with HU in medical CT. In CBCT, image grey shades range between black and white, and the displayed shades can be arbitrarily limited to a large or small window within a contrast control scale. The windowing can be raised or lowered depending upon the absorption value of the material of interest, but at the same point the examiner must be able to decide which window level and width will most accurately represent the anatomic truth of a tissue under examination.

Ct Scan Download
Without a concise designation of the windowing that was used to evaluate a patient’s image, it is impossible to reproduce the measurements and also to compare results between studies. Future studies should render the diagnostic accuracy of measurements in images where windowing varied.The orientation plane for generation of the sections before measuring a grafted bone is another important issue. The DICOM data set can be accessed in different manners, and the operator can visualize it by going through a determined stack of sections. The 3D image can be reformatted and 2D images generated based on the 3D data set, allowing the operator to scroll through the 2D images in any plane or direction, and also in different depths, depending on section thickness. The generated sections will completely depend on the orientation planes. Knowing how the patient’s head is oriented and in which direction the slices will be generated is a “sine qua non”.
Dicom Sample File
To facilitate image comparison over time, there are ways to superimpose CBCT data sets obtained from the same region, assuring that the images are generated from the same position. Reliable and accurate landmark-based superimposition techniques for evaluating changes over time have not been established yet, but there is focus on the issue. In our review, the included papers aimed only at the anatomic guidelines to access a determined ROI and offered no information about recreating the same ROI in different images. Without this information a study cannot be reproduced, and the scientific value of papers that do not address this parameter can be contested since without the plane definition, the same ROI can be shown in diverse forms, many of them creating “contaminated” images of the area to be measured. In some cases, image signal-to-noise ratio may dictate the selection of section thickness; the thicker the sections the higher the signal-to-noise ratio in the images.We also addressed the cross-sectional section thickness and the inter-section interval (the distance between adjacent cross-sectional images), directly connected to the number of evaluated sections from each grafted site. Some clinicians believe that thinner, more closely approximated cross-sectional sections provide more accurate information since they are more prone to display important diagnostic features of a disease or condition , while thicker sections might show the superimposition of other structures, disturbing the evaluation of the ROI.
It may also be possible to affirm that the more sections, the more precise the data extracted from the data set since the appearance of the reconstructed images (as reflected by differences in bone linear measurements) will be closer to the anatomical reality.From our results, it is clear that software used for bone graft measurements in CBCT image sections must allow user control of the addressed parameters (windowing, plane orientation, slice thickness, and inter-slice interval). It must be a demand that authors specify the setting of these parameters, including the image acquisition protocol, image reconstruction, and image generation information, in order to allow reproduction and comparability among studies. ConclusionThe parameters for image acquisition and reconstruction were not addressed in enough detail in the studies selected for this review, compromising their value. Based on our experiment, it can be concluded that CBCT images differ depending on windowing settings, plane definition, and number and thickness of sections, likely to influence measurement outcomes. We suggest that software to be used for bone measurements in CBCT images must include the possibility for controlling these variables, and that future studies describe in detail the used settings.




